Why do different etiologies follow different pattern of Necrosis to liver zones.
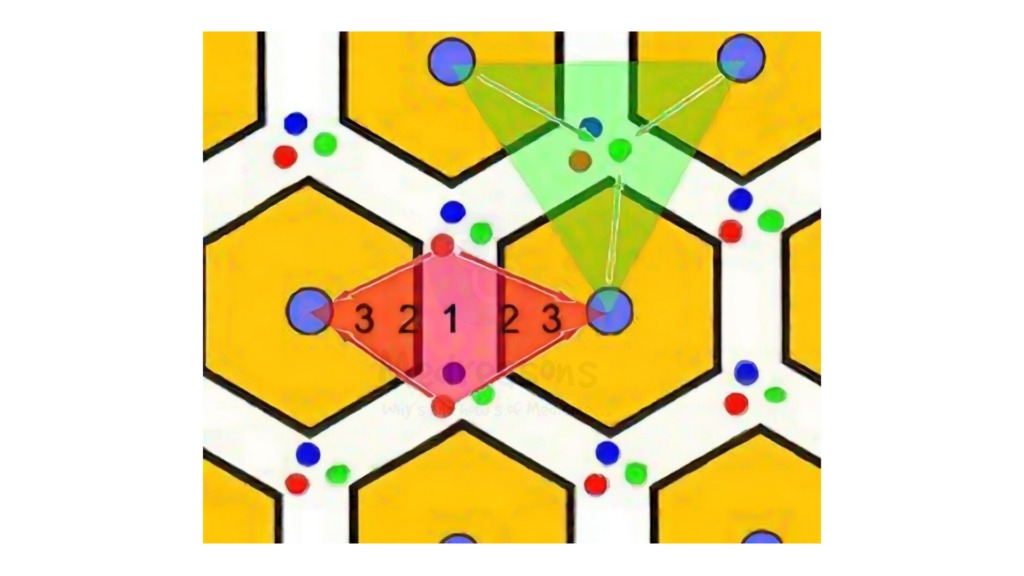
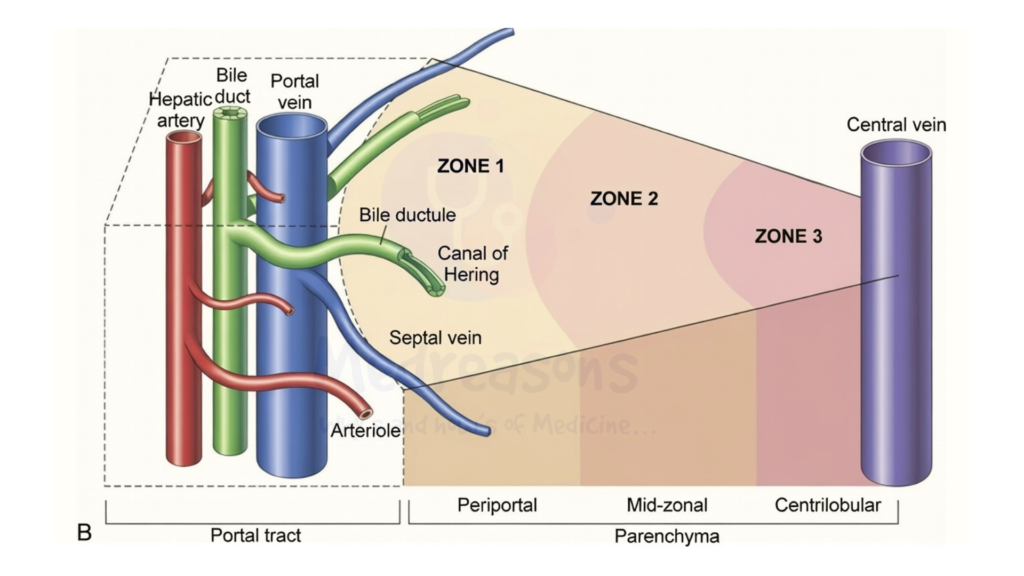
This topic highlights the fascinating Hepatic zonation — the functional division of the liver lobule into three zones based on blood flow, oxygen gradient, and metabolic specialization:
- Zone 1 (Periportal): Closest to incoming oxygenated blood from the portal vein and hepatic artery; high in oxidative metabolism.
- Zone 2 (Midzonal): Intermediate area.
- Zone 3 (Centrilobular): Farthest from oxygen source, around the central vein; lowest oxygen, highest in drug-metabolizing enzymes (e.g., cytochrome P450).
Different causes of liver injury exploit these zonal differences in blood supply, oxygen levels, enzyme expression, and metabolic roles, leading to characteristic necrosis patterns.
Additionally, the concept of hepatic zones helps in understanding the differential impact of various liver diseases.
Understanding Liver Zonation and Necrosis Patterns
The liver lobule is organized into acinar zones with a porto-central blood flow gradient. Oxygen and nutrients are highest in Zone 1 (periportal) and lowest in Zone 3 (centrilobular). Hepatocytes in each zone express different genes and enzymes, creating metabolic specialization. Understanding hepatic zones is crucial in studying liver function and its intricate dynamics.
This zonation explains why liver injury is rarely uniform — toxins, viruses, ischemia, or congestion target specific zones based on:
– Oxygen gradient → Zone 3 is most vulnerable to hypoxia.
– Enzyme distribution → Drug-metabolizing CYPs are concentrated in Zone 3.
– Blood flow and immune access → Zone 1 receives incoming pathogens/immune cells first.
– Direct viral tropism or inflammatory patterns.
Centrilobular Necrosis (Zone 3) – Most Common Pattern
Zone 3 hepatocytes receive the least oxygen and have the highest levels of cytochrome P450 enzymes, making them prone to hypoxic and toxic injuries.
Common etiologies and mechanisms:
– **Chronic venous congestion (e.g., cardiac failure / congestive hepatopathy)**
Backward pressure from right heart failure causes sinusoidal congestion and reduced perfusion → hypoxia → centrilobular dropout/necrosis. Often with sinusoidal dilation and red blood cell extravasation.
– **Acetaminophen (paracetamol) toxicity**
Overdose → excess NAPQI (toxic metabolite) produced via CYP2E1 (concentrated in Zone 3) → glutathione depletion → oxidative stress, mitochondrial damage, peroxynitrite formation → hepatocyte necrosis. Classic centrilobular pattern; Zone 3 vulnerability due to high bioactivation enzymes and low oxygen.
– **Budd-Chiari syndrome**
Hepatic vein outflow obstruction → congestion and ischemia → centrilobular necrosis, often progressing to fibrosis.
– **Ischemia / shock liver**
Hypotension or hypoperfusion → reduced oxygen delivery to distal Zone 3 → coagulative necrosis.
– **Alcoholic hepatitis**
Alcohol metabolism via CYP2E1 in Zone 3 → oxidative stress, inflammation, ballooning, Mallory bodies, and centrilobular predominance.
These injuries often start in Zone 3 and may extend if severe.
Midzonal Necrosis (Zone 2)
Less common; intermediate zone affected in specific scenarios.
– **Yellow fever**
Direct viral infection of hepatocytes → midzonal injury with Councilman bodies (apoptotic hepatocytes), steatosis, and minimal inflammation. Virus tropism and in-situ inflammatory response target Zone 2; characteristic of flavivirus pathology.
Midzonal pattern can rarely occur post-shock or in regenerating livers after centrilobular injury.
Periportal Necrosis (Zone 1)
Zone 1 receives oxygenated blood first and is exposed to incoming antigens/pathogens.
– **Viral hepatitis (e.g., acute hepatitis A, B, or others)**
Immune-mediated attack (cytotoxic T cells) targets infected hepatocytes → interface hepatitis / piecemeal necrosis at portal-parenchymal junction. Inflammation spills from portal tracts into Zone 1. Spotty necrosis may occur lobularly, but periportal predominance reflects immune access via portal inflow.
Periportal injury is also seen in some autoimmune or drug-induced cases, but viral hepatitis classically shows this pattern.
### Key Takeaways: Why the Patterns Differ
| Zone | Key Vulnerabilities | Common Causes | Mechanism Summary |
|————|———————————————-|—————————————-|————————————————|
| Zone 3 (Centrilobular) | Lowest oxygen, highest CYP450 enzymes | Acetaminophen, ischemia, cardiac failure, alcohol, Budd-Chiari | Hypoxia + bioactivation of toxins → oxidative stress + mitochondrial failure |
| Zone 2 (Midzonal) | Intermediate; specific viral tropism | Yellow fever | Direct viral cytopathy + localized inflammation |
| Zone 1 (Periportal) | First exposure to portal blood/antigens | Viral hepatitis | Immune-mediated attack on incoming infected cells |
These patterns arise from evolutionary adaptations: Zone 3 specializes in detoxification but at the cost of hypoxia vulnerability; Zone 1 handles oxidative processes and immune surveillance.
Understanding zonal necrosis aids diagnosis, predicts progression, and guides therapy (e.g., N-acetylcysteine for acetaminophen targeting glutathione in Zone 3).
